Have you been diagnosed with Endometrial Cancer (EC)? Discover a treatment option for certain types of EC
You are about to leave a GSK website
You are about to leave a GSK website. By clicking this link, you will be taken to a website that is independent from GSK. The site you are linking to is not controlled or endorsed by GSK and GSK is not responsible for its content.
Staying Silent Can Leave You at Risk for Endometrial Cancer
Don’t Be Embarrassed About Your Gynecologic Health
We've never been embarrassed before. We've never stumbled in front of a group of people, or started speaking and lost our train of thought, or walked around all day with an unbuttoned button showing the world what style bra we had on... Of course, we're kidding. We've all been there. And while the thought of talking openly about your private parts may make you wince, we're telling you right now: YOU SHOULD NEVER BE EMBARRASSED SHARING CONCERNS ABOUT YOUR BODY!
Endometrial Cancer (EC) is serious and mostly affects
women over 45. However, if you have a uterus, you
may be at risk.
MOM!
Mothers and daughters often have a special connection. OK, maybe not during those delightful teenage years! Here is a story of a mother and daughter and how their relationship changes over time, awkward moments and all.
Let's Keep the Conversation Going
What Is Endometrial Cancer (EC)?
It doesn’t quite roll off the tongue, and you may have never heard of it. So what exactly is EC? It’s a cancer that begins in the endometrium, the tissue that lines the uterus.
EC is the most common form of gynecologic cancer in the US, with 62,000 new cases estimated to be diagnosed in 2025. That’s more than 160 women every single day—about one every 9 minutes—receiving a life-altering diagnosis. In the US alone, nearly 12,500 women are estimated to die from EC in 2025.
Yeah, it’s serious, so let’s get you up to speed on what to keep an eye on!
Postmenopausal bleeding is often associated with benign conditions as well, like endometrial polyps or use of hormone therapy. If you have abnormal bleeding, it’s recommended that you see your doctor to determine the cause.
What Exactly Is Menopause?
Yeah, we get it, menopause is not something most people look forward to. That doesn't mean it has to be the biological roller coaster your aunt Martha terrified you about. There are many misconceptions about menopause and the changes it brings.
Many people use the term menopause to refer to the time when a woman's menstrual periods stop. However, there are different stages of menopause, which we’ve defined below along with some other important terms. To make things a little more clear, we’ll use the term Transition to Menopause to refer to the full experience including perimenopause and postmenopause.
What the Heck Do These Symptoms Mean?
When changes to your body happen, you may ask yourself, "Is this normal?" This chart should help give you an idea of what you should expect and when something needs extra attention—when you need to reach out to your gynecologist.
TRANSITION TO MENOPAUSE vs EC:
Are These Symptoms? What Could They Mean?
| SYMPTOM | TRANSITION TO MENOPAUSE | EC | WHAT IT COULD MEAN |
|---|---|---|---|
| Irregular vaginal bleeding | Yes | Yes | Irregular bleeding in perimenopause and any postmenopausal bleeding could be a sign of something wrong, including EC, and should be discussed with your doctor. |
| Pelvic pain | Occasionally | Yes | Persistent pelvic pain (soreness, discomfort, or a feeling of fullness in the pelvis) is less common in the Transition to Menopause and may indicate EC. |
| Unintentional Weight loss | No | Yes | Weight gain is common during the Transition to Menopause, while unintentional weight loss (losing weight despite no changes in diet or lifestyle) can be a sign of EC. |
| Weight gain | Yes | Possibly | Weight gain is common during the Transition to Menopause; however, obesity is a significant risk factor for EC. |
| Vaginal discharge | Yes | Yes | While changes in discharge can occur during the Transition to Menopause, abnormal discharge may be a sign of EC. |
| Gastrointestinal symptoms | Yes | Yes | Older women with EC had a higher incidence of gastrointestinal symptoms (bloating, constipation, and diarrhea) than similar women without cancer. |
Important Terms to Know
| Perimenopause | Refers to the body’s natural Transition to Menopause, usually 3 to 5 years before menopause, and is often marked by many of the symptoms of menopause |
| Menopause | The point in time when a person has gone 12 straight months without a menstrual period, marking the end of reproductive years |
| Postmenopause | Refers to the time after menopause |
| Hormone | A substance (such as estrogen and progesterone) produced in the body and transported to control specific cells, tissues, or organs |
| Estrogen | Often called the female sex hormone. In women, estrogen levels normally cycle on a monthly schedule to regulate menstruation and prepare the body for fertilization and reproduction. Estrogen may promote the growth of cancer cells |
| Progesterone | A female sex hormone released during every menstrual cycle to prepare the uterus for pregnancy and the breasts for milk production |
| Cowden Syndrome | A condition in which noncancerous growths appear on the skin and around the mouth |
| Lynch Syndrome | An inherited condition that increases the risk of certain types of cancer |
| Polycystic Ovary Syndrome | A problem with hormones where small sacs of fluid develop along the outer edge of the ovary |
Three Key Symptoms of EC
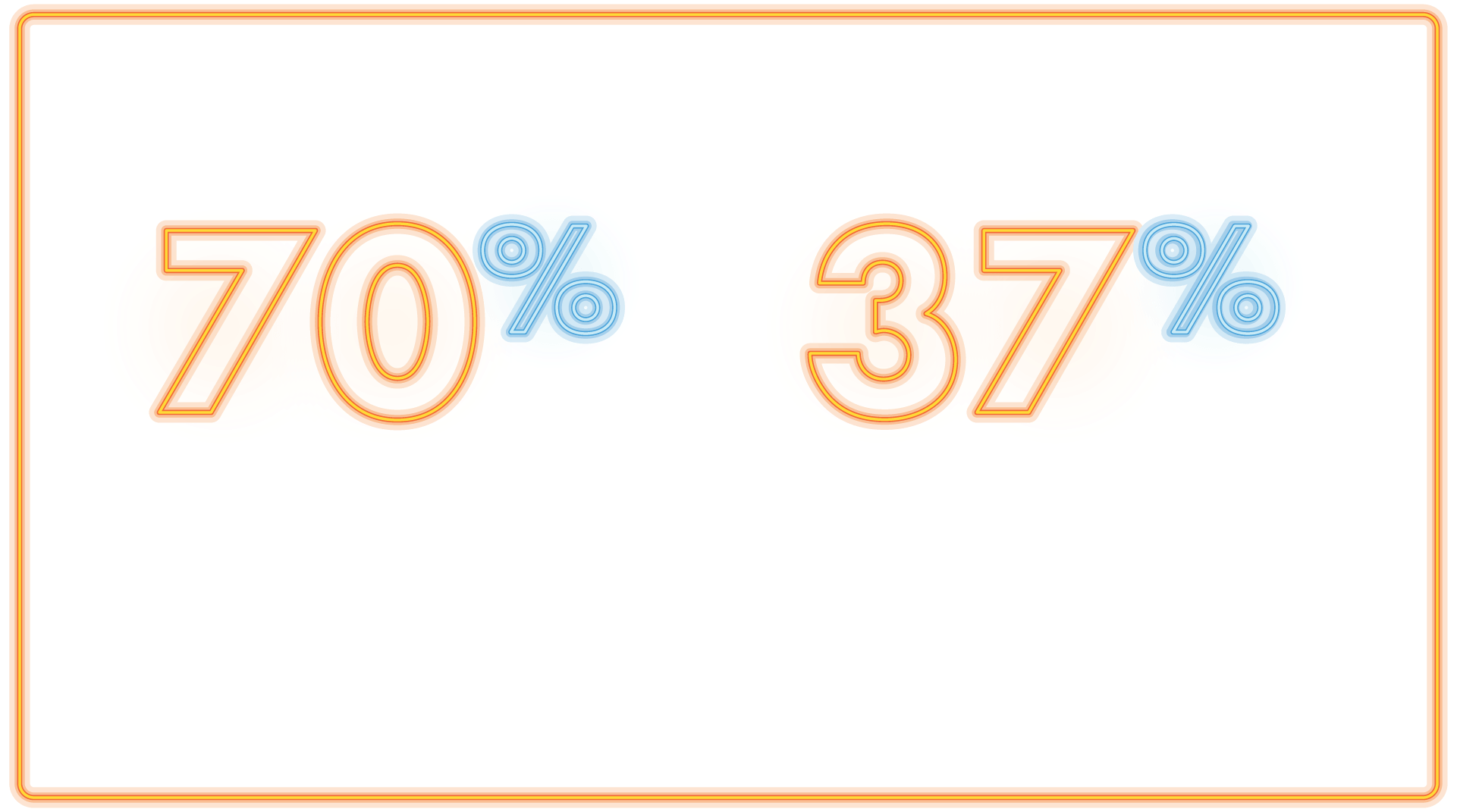
- About 90% of women with EC experienced abnormal bleeding
- Approximately 9% of women who saw a doctor for postmenopausal bleeding later received a diagnosis of endometrial cancer
- Pelvic pain and spotting aren’t just symptoms of the Transition to Menopause; they may be signs of EC or other conditions

Abnormal Vaginal Bleeding
While irregular bleeding is common during perimenopause, if you experience that you should tell your healthcare team immediately, as well as if you experience even light spotting or abnormal bleeding after menopause.

New or Unusual Discharge
The Transition to Menopause can cause dryness, but abnormal vaginal discharge is not typical and may signal a problem like EC.
Persistent Pelvic Pain
The Transition to Menopause might bring general discomfort, but ongoing pelvic pressure, bloating, or pain—especially if it’s new—shouldn’t be dismissed.

If symptoms during your Transition to Menopause feel unusual or abnormal, it may be more than menopause. Trust your intuition. Listen to your body and talk about it.

It’s time to learn about risk factors for EC.
Many EC risk factors—like obesity and having an early first period and/or late menopause—are linked to excess exposure to estrogen without enough progesterone to balance it. This hormonal imbalance can cause the lining of the uterus to build up too much, which over time may lead to cancer. Let’s see what else you need to be aware of:
- If you’re menopausal and taking estrogen-only hormonal replacement therapy to alleviate symptoms, you may be at an increased risk of developing EC
- Higher body weight and diabetes may put you at a higher risk for EC
- In the US, 57% of cases of EC are attributed to obesity
- Obesity is more strongly associated with EC than any other cancer type
- Additional risk factors include:
- Advanced age
- Early menarche (first period) and/or late menopause
- Family history
- No history of pregnancy
- Cowden syndrome
- Lynch syndrome
- Polycystic ovary syndrome
Black and Native American people face the highest rates of new cases of EC in the US. So speak up for yourself and your community!